INTRODUCTION
Ligneous conjunctivitis is a recurrent, rare form of chronic bilateral conjunctivitis characterized by the development of fibrin-rich, firm, wood-like pseudomembranous lesions, particularly on the tarsal conjunctiva. Plasminogen deficiency is a common cause of ligneous conjunctivitis(1-4); this deficiency can affect not only the conjunctiva but also the other mucous membranes of the body. such as those of the oral mucosa, nasopharynx, trachea, female genital tract, and duodenum. Congenital hydrocephaly may develop in some patients with plasminogen deficiency(5).
The management of ligneous conjunctivitis is difficult because of a lack of both therapeutic products and recommendations for appropriate substitution therapy. Several therapeutic modalities have been reported for the treatment of ligneous conjunctivitis and prevention of recurrences. However, no consensus has been gained on the treatment regimen(1,3). The efficacy of topically applied fresh frozen plasma (FFP) together with subconjunctival FFP has been previously demonstrated in a patient with ligneous conjunctivitis(6).
To the best of our knowledge, this study is the first to demonstrate the efficacy of topical FFP treatment alone without either subconjunctival application or systemic therapy in an infant with ligneous conjunctivitis.
CASE REPORT
In this report, all experiments were performed in accordance with the Declaration of Helsinki and with the approval of Institutional Review Board. Informed consent was obtained from the patient's parents.
A 6-month-old female infant presented to our clinic with a 4-month history of bilateral eyelid swelling, yellowish-white membranes under both lids, and mucoid ocular discharge (Figure 1). No other pathology was detected in the anterior or posterior ocular segments. The girl was born at 32 weeks of gestation with a birth weight of 1640 g. Further, her past history revealed congenital hydrocephalus with spontaneous resolution, and her parents were first cousins. Her 32-year-old aunt had similar ocular problems that were undiagnosed. The aunt also had a history of membranous gingivitis and had lost her teeth in the second decade of her life. The patient's first cousin (maternal aunt's 2-month-old boy) also had a history of congenital hydrocephalus.

Figure 1 Conjunctival membranes on the lower and upper eyelids in the patient with ligneous conjunctivitis before treatment.
We excised the conjunctival membranes and administered topical netilmicin preservative-free eye drops (SIFI S.P.A, Italy) 4 times daily, sodium hyaluronate preservative-free eye drops (SIFI S.P.A, Italy) 4 times daily, and dexamethasone ointment (Alcon Couvreur, Belgian) 2 times daily for the first two postoperative days. Serological and microbiological examinations for cytomegalovirus, Epstein-Barr virus, human immunodeficiency virus, rubella virus, Toxoplasma gondii, mycoplasma pneumonia, Chlamydia trachomatis, Treponema pallidum, and Corynebacterium diphtheria were negative. Her blood group was O positive. Histopathological examination of the excised conjunctival membranes exhibited a massive fibrin exudation with a disrupted epithelium, inflammatory cellular infiltration, and moderate leukocyte infiltration (Figure 2), confirming ligneous conjunctivitis. All clinical signs and her family history indicated plasminogen deficiency. We measured her plasminogen activity at 24% (normal range, 80%-120%); her aunt's and cousin's plasminogen activities were 16%.
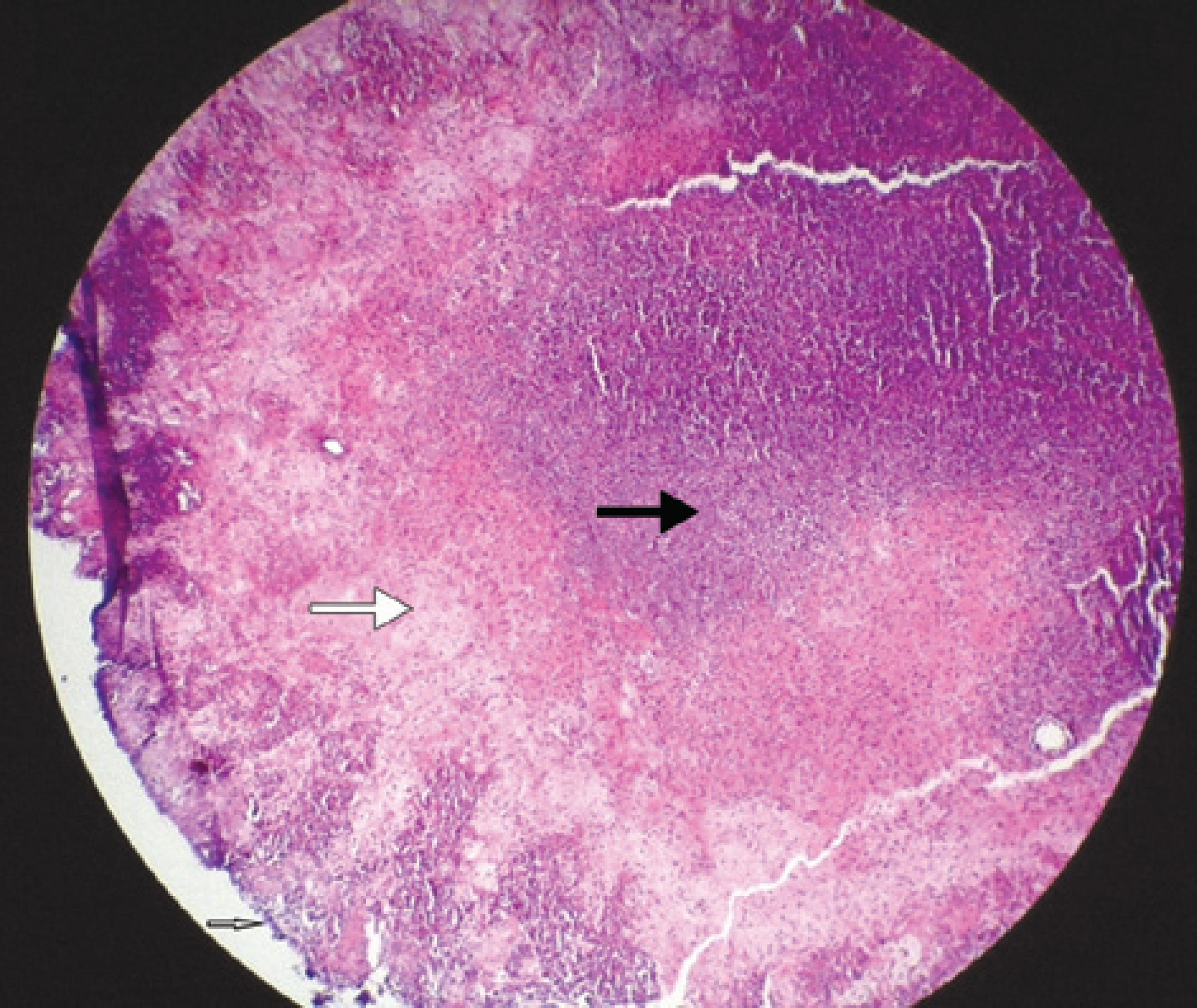
Figure 2 Histopathology of the conjunctival membranes (white arrow: disrupted epithelium; large white arrow: massive exudation of fibrin; black arrow: inflammatory cellular infiltration).
We referred the patient to a pediatric hematology clinic, and they did not recommend any systemic treatment. Further, we examined the patient daily and recognized new membrane formation on the lower eyelids on the third postoperative day. We decided to use topical FFP as plasminogen concentrates for use as eye drops are not yet commercially available. We then obtained plasma from a O negative donor with a normal plasminogen level. Sterile drop bottles with 3-ml plasma were frozen at -40°C, and each bottle was thawed for daily use and refrigerated at 4°C for 24 h. The topical FFP eye drops were used 6 times daily for 6 weeks; no recurrence was observed during this period. Furthermore, the patient's parents abruptly discontinued the treatment. On the 15th day after the treatment discontinuation, the patient presented to our clinic with bilateral ligneous conjunctivitis. We treated her with topical FFP 6 times daily, netilmicin and collyrium (SIFI S.P.A, Italy) 4 times daily, and topical dexamethasone ointment (Alcon Couvreur, Belgian) 2 times daily for 1 week. The treatment was then continued with only topical FFP 6 times daily. No recurrence was observed during the 3-month follow-up period (Figure 3).
DISCUSSION
In this report, we aimed to demonstrate the successful outcome of topical FFP application in an infant with ligneous conjunctivitis; topical FFP without any systemic treatment prevented new or recurrent conjunctival membrane formation after the excision of the conjunctival membranes. Several treatment approaches have been recently reported for treating ligneous conjunctivitis and for preventing the recurrence of the membranes. However, no treatment modality has been accepted(6-9). The treatment regimens generally focus on plasminogen since the etiology of the disease has been clarified, and Schott et al. (1998) have successfully used it(10). Despite studies revealing the efficacy of plasminogen, it is not commercially available.
Tabbara has demonstrated the efficacy of topically and subconjunctivally applied FFP in patients with ligneous conjunctivitis(6). Pergantou et al. and Gürlü et al. have declared that the simultaneous application of systemic and topical FFP was effective in treating ligneous conjunctivitis and preventing recurrences(2,3).
The risks of FFP include hemolysis, infections, transfusion-related acute lung injury, allergic reactions, and anaphylaxis. Systemic treatment also requires hospitalization and intravenous application. Another drawback of FFP is its short half-life(2,3,7,8). To minimize these unwanted effects and difficulties, we decided to use only topical FFP as eye drops in this patient. Our patient showed a good response to topical FFP treatment, and the membranes have not recurred detected while using it.




 English PDF
English PDF
 Print
Print
 Send this article by email
Send this article by email
 How to cite this article
How to cite this article
 Submit a comment
Submit a comment
 Mendeley
Mendeley
 Scielo
Scielo
 Pocket
Pocket
 Share on Linkedin
Share on Linkedin

