

Caio Scocco1; Sérgio Kwitko2; Samuel Rymer3; Diane Marinho2; Francisco Bocaccio3; Rodrigo Lindenmeyer2
DOI: 10.1590/S0004-27492008000600003
ABSTRACT
PURPOSE: To evaluate the long-term outcome of HLA-matched lr-CLAL for bilateral ocular surface disorders. METHODS: A retrospective, non-comparative interventional case series study of 39 eyes of 32 patients with bilateral surface disorders and clinical diagnosis of limbal stem cell deficiency who underwent HLA-matched lr-CLAL. Visual acuity (VA), ambulatory vision (> 20/200) and ocular surface stability were evaluated as main outcomes. Donor limbus was obtained from a sibling or a parent of the patient, after an appropriate Class I and II HLA match. RESULTS: One year after surgery, VA improved in 46.2%, ambulatory vision was achieved in 48.7% and a stable corneal surface was achieved in 84.6% of the eyes. At the final follow-up (mean, 48.7 ± 30.6 months), 66.6% of the eyes that had gained VA one year after surgery maintained an improved VA (p=0.28), 94.7% of eyes that had achieved ambulatory vision one year after surgery maintained 20/200 or better (p<0.001) and 93.9% still had a stable corneal surface (p=0.043) at the final follow-up. CONCLUSIONS: HLA-matched lr-CLAL can be an adequate method of treatment for bilateral ocular surface disorders, with a reasonable percentage of success of long-term results.
Keywords: Transplantation, homologous; Cornea limbus; Living donors; HLA antigens
RESUMO
OBJETIVO: Avaliar os resultados em longo prazo do transplante alogênico inter vivo de limbo conjuntival para doenças bilaterais da superfície ocular com compatibilidade HLA doador-receptor. MÉTODOS: Estudo retrospectivo, não comparativo e intervencionista de 39 olhos de 32 pacientes submetidos a transplante alogênico de limbo com compatibilidade HLA e diagnóstico de deficiência límbica. Foram analisados como desfechos principais acuidade visual, visão ambulatorial (> 20/200) e estabilidade da superfície ocular. Limbo doador foi obtido de parentes do paciente após estudo de compatibilidade HLA classe I e II. RESULTADOS: Com um ano de pós-operatório, a acuidade visual melhorou em 46,2%, visão ambulatorial foi atingida em 48,7% e estabilidade da superfície corneana em 84,6% dos pacientes. Ao final do seguimento (média, 48,7 ± 30,6 meses), 66,6% dos olhos que haviam ganho acuidade visual um ano após a cirurgia mantiveram esta melhora (p=0,28), 94,7% dos olhos que haviam alcançado visão ambulatorial um ano após a cirurgia mantiveram visão de 20/200 ou melhor (p<0,001) e 93,9% ainda tinham superfície corneana estável (p=0,043) ao final do seguimento. CONCLUSÕES: O transplante alogênico inter vivo de limbo conjuntival com compatibilidade HLA revelou-se método adequado no tratamento de doenças bilaterais da superfície ocular, com uma porcentagem significativa de sucesso a longo-prazo.
Descritores: Transplante homólogo; Limbo da córnea; Doadores vivos; HLA antígenos
ORIGINAL ARTICLE
HLA-matched living-related conjunctival limbal allograft for bilateral ocular surface disorders: long-term results
Transplante alogênico inter vivo de limbo conjuntival com pareamento HLA em doenças bilaterais da superfície ocular: resultados em longo prazo
Caio ScoccoI; Sérgio KwitkoII; Samuel RymerIII; Diane MarinhoIV; Francisco BocaccioV; Rodrigo LindenmeyerVI
IEstagiário do Setor de Retina e Vítreo do Hospital de Olhos do Paraná - Curitiba (PR) - Brasil
IIDoutor, Preceptor da Residência do Serviço de Oftalmologia do Hospital de Clínicas de Porto Alegre (RS) - Brasil
IIIDoutor, Professor do Departamento de Oftalmologia da Universidade Federal do Rio Grande do Sul - UFRGS - Porto Alegre (RS) - Brasil
IVDoutora, Preceptora da Residência do Serviço de Oftalmologia do Hospital de Clínicas de Porto Alegre (RS) - Brasil
VProfessor do Departamento de Oftalmologia da UFRGS - Porto Alegre (RS) - Brasil
VIPreceptor da Residência do Serviço de Oftalmologia do Hospital de Clínicas de Porto Alegre - (RS) - Brasil
ABSTRACT
PURPOSE: To evaluate the long-term outcome of HLA-matched lr-CLAL for bilateral ocular surface disorders.
METHODS: A retrospective, non-comparative interventional case series study of 39 eyes of 32 patients with bilateral surface disorders and clinical diagnosis of limbal stem cell deficiency who underwent HLA-matched lr-CLAL. Visual acuity (VA), ambulatory vision (> 20/200) and ocular surface stability were evaluated as main outcomes. Donor limbus was obtained from a sibling or a parent of the patient, after an appropriate Class I and II HLA match.
RESULTS: One year after surgery, VA improved in 46.2%, ambulatory vision was achieved in 48.7% and a stable corneal surface was achieved in 84.6% of the eyes. At the final follow-up (mean, 48.7 ± 30.6 months), 66.6% of the eyes that had gained VA one year after surgery maintained an improved VA (p=0.28), 94.7% of eyes that had achieved ambulatory vision one year after surgery maintained 20/200 or better (p<0.001) and 93.9% still had a stable corneal surface (p=0.043) at the final follow-up.
CONCLUSIONS: HLA-matched lr-CLAL can be an adequate method of treatment for bilateral ocular surface disorders, with a reasonable percentage of success of long-term results.
Keywords: Transplantation, homologous/methods; Cornea limbus/surgery; Living donors; HLA antigens
RESUMO
OBJETIVO: Avaliar os resultados em longo prazo do transplante alogênico inter vivo de limbo conjuntival para doenças bilaterais da superfície ocular com compatibilidade HLA doador-receptor.
MÉTODOS: Estudo retrospectivo, não comparativo e intervencionista de 39 olhos de 32 pacientes submetidos a transplante alogênico de limbo com compatibilidade HLA e diagnóstico de deficiência límbica. Foram analisados como desfechos principais acuidade visual, visão ambulatorial (> 20/200) e estabilidade da superfície ocular. Limbo doador foi obtido de parentes do paciente após estudo de compatibilidade HLA classe I e II.
RESULTADOS: Com um ano de pós-operatório, a acuidade visual melhorou em 46,2%, visão ambulatorial foi atingida em 48,7% e estabilidade da superfície corneana em 84,6% dos pacientes. Ao final do seguimento (média, 48,7 ± 30,6 meses), 66,6% dos olhos que haviam ganho acuidade visual um ano após a cirurgia mantiveram esta melhora (p=0,28), 94,7% dos olhos que haviam alcançado visão ambulatorial um ano após a cirurgia mantiveram visão de 20/200 ou melhor (p<0,001) e 93,9% ainda tinham superfície corneana estável (p=0,043) ao final do seguimento.
CONCLUSÕES: O transplante alogênico inter vivo de limbo conjuntival com compatibilidade HLA revelou-se método adequado no tratamento de doenças bilaterais da superfície ocular, com uma porcentagem significativa de sucesso a longo-prazo.
Descritores: Transplante homólogo/métodos; Limbo da córnea/cirurgia; Doadores vivos; HLA antígenos
INTRODUCTION
Extensive experimental work demonstrated that limbal epithelial cells, the "stem cells", are responsible for corneal epithelial differentiation and proliferation, and contribute to a regular optical and stable corneal surface. When these cells are damaged, as in severe alkali burns, a process of corneal conjunctivalization and vascularization begins. This can lead to a corneal scar, or to persistent corneal epithelial defects, trophic ulcers, corneal melt and even perforation(1-5).
Autologous conjunctival transplantation was first suggested in 1977 for cases of severe unilateral alkali burn(1). Further studies demonstrated a higher success rate with limbal transplantation for ocular surface diseases, which is related to the presence of a healthy limbal epithelium in the unaffected fellow eye(5-6).
When, however, patients have bilateral surface involvement, such as in bilateral burns, Stevens-Johnson syndrome, Lyell's syndrome, ocular cicatricial pemphigoid, trachoma, aniridia and ectodermal dysplasia, there is no healthy limbal epithelium in the fellow eye. For these cases, Thoft suggested, in 1984, transplantation of non-preserved corneal limbal epithelia from fresh donor cadaver eyes, a surgery the author named "keratoepithelioplasty"(7).
Furthermore in 1985, an author reported encouraging results of allograft limbal transplantation in nonhuman primates(8). Several authors(9-13) have also reported good results performing allograft limbal transplantation from non-matched cadaver donor eyes, but with strong systemic immunosuppression. We have reported encouraging preliminary results of allograft conjunctival limbal transplantation for bilateral surface disorders, where donor limbus was obtained from HLA-matched relatives, without systemic immunosuppression(14). Recently, other authors(15-17) also showed good results of limbal transplantation from either HLA-matched relatives or cadaver donor eyes with the use of immunosuppression.
However, stability of results is still a challenge in these cases, with loss of good initial results over time(18-19).
We present herein the long-term results of a retrospective study of HLA-matched living-related conjunctival limbal allografts (lr-CLAL) in 39 eyes of 32 patients with bilateral surface disorders.
METHODS
Thirty-nine eyes of 32 patients with bilateral ocular surface diseases that underwent HLA-matched lr-CLAL and at least 18 months of follow-up were retrospectively reviewed and included in the study. The protocol was approved by the Ethics Research Committee of the Hospital de Clínicas de Porto Alegre.
All eyes had bilateral ocular surface diseases that were unresponsive to medical therapy. All patients had one or more of the following signs of limbal deficiency: persistent epithelial defect, trophic corneal ulcer, corneal necrosis, corneal conjunctivalization, and/or corneal scar with intense vascularization, due to the following causes of bilateral ocular surface diseases: Stevens-Jonhson syndrome in 14 eyes, bilateral alkali burns in 12 eyes, Lyell's syndrome in 5 eyes, ectodermal dysplasia in 3 eyes, limbal tumors in 2 eyes, multiple pterygium surgery in 2 eyes, and ocular cicatricial pemphigoid in 1 eye.
Patients in use of systemic immunossupression were excluded from the study.
Eyes were classified according to the classification of Holland, Gomes and Shwartz(19), to analyze and better compare the results (Table 1).
Donor limbus was obtained from a sibling of the patient or, if they had none, from one of their parents, after an appropriate Class I and II HLA match.
Snellen visual acuity (VA), ambulatory vision - defined when the best-corrected visual acuity was 20/200 or better(20) - and surface stability - measured as presence or absence of corneal epithelial defect where fluorescein drop examinations were evaluated pre- and postoperatively as main outcomes. Corneal transparency - measured as totally transparent cornea, mild opacity not obscuring iris details, mild opacity obscuring iris details or totally opaque cornea - and neovascularization - measured in millimeters through the visual axis - were evaluated as secondary outcomes.
Limbal allograft rejection was considered when either an ischemic graft was present or intense vessel dilation adjacent to the graft was seen(12,21). Primary failure was considered when a poor adherence of the graft was noted during the first 14 days after surgery. Rejection cases were treated with steroid drops. Failure cases were treated with a new graft from the same or another donor when possible.
Survival of transplanted limbal epithelial stem cells was defined by duration of maintaining a normal corneal epithelial phenotype or, at least, abscence of epithelial defects after surgery. Survival of visual acuity (VA) was defined as maintenance of a stable or improved VA after surgery.
Serological analysis of HLA antigens and cross-matching was carried out as previously reported(14).
Surgical technique
We used the surgical technique described previously by other authors(6) and modified by us(14). Either general or peribulbar anesthesia was used in all recipients. Subconjunctival anesthesia was used in all donors. All surgeries were performed under a surgical microscope (Topcon OMS-600 or OMS-610, Tokyo, Japan).
One or two flaps of donor conjunctival limbus, depending on the severity of disease in the recipient, were prepared. A 5 x 8 mm conjunctival flap, including limbal area, was prepared with sharp Wescott scissors beginning at the conjunctiva far from the limbus, and dissecting it toward the limbus with a crescent knife (Allergan, Irvine, CA). The limbal area was cut with sharp Vannas scissors, without making any peripheral keratectomy. This tissue was then removed from the donor eye and kept on a moist surface until the recipient eye was prepared. Care was taken to keep the donor conjunctiva moist with balanced salt solution. No sutures were placed to close the donor site.
A 360º peritomy and either a superficial keratectomy or only epithelial removal, depending on corneal opacity and thickness, were performed on the recipient eye. Donor limbal flaps were sutured onto the recipient eye, taking care to keep the limbal side of the flap facing the recipient limbus. The donor flap was sutured to the recipient eye with two 10.0 nylon buried sutures at the cornea, and two 8.0 vicryl sutures at the conjunctival side.
In those patients where amniotic membrane transplantation (AMT) was added to the lr-CLAL, the amniotic membrane was sutured first to the episcleral and corneal surface and the lr-CLAL was placed over it. Amniotic membrane was preserved according to the technique previously described by other authors(22).
Statistical Analysis
Last Observation Carried Forward (LOCF)(23) was used, and qualitative variables were expressed as percentages relative to the total number of cases or to a specific subgroup to which it belonged. Statistical analysis of the results was performed by Pearson's chi-square, with continuity correction when on 2x2 tables, and by Fisher's exact test. Kaplan-Meier survival analysis was performed to evaluate two outcome measures after last surgery: visual acuity (VA) and ocular surface stability. A P value less than 0.05 was considered statistically significant.
RESULTS
Table 2 shows preoperative and postoperative data. Patients' mean age was 33.62 ± 18.95 years (minimum 2, maximum 86 years).
HLA compatibility was identical in 15 donor-recipient pairs (38.5%), had a 75% match in 4 pairs (10.2%), and had 50% identity (haplo-identical HLA) in 20 pairs (51.3%). A second lr-CLAL was necessary in 13 eyes (33.3%), mean time of 22.3 ± 8.95 months, due to an unstable ocular surface after the first lr-CLAL. Amniotic membrane transplantation (AMT) was associated with lr-CLAL in 7 eyes (17.9%). Eight eyes (20.5%) were also submitted to a penetrating keratoplasty (PKP), 1 eye at the same time of lr-CLAL, and 7 eyes 19.6 ± 17.8 months after the lr-CLAL.
There were no intraoperative complications, such as perforation, and no epithelial healing problems in donor eyes. One donor eye developed granulomatous formation at the conjunctival site of limbal donation, which was surgically removed; histology revealed an unspecific inflammatory reaction.
One week after surgery, each limbal graft was well adherent to the recipient bed in all eyes.
One year after surgery, visual acuity improved in 18 (46.2%) of the eyes, ambulatory vision (20/200 or better) was achieved in 19 (48.7%) eyes and a stable corneal surface was achieved in 33 (84.6%). Corneal transparency improved in 22 (56.4%) and corneal vascularization was reduced in 23 (59%).
All eyes were followed up for more than one year, with a mean follow-up period of 48.7 ± 30.6 months (minimum 18 months, maximum 121 months).
At the final follow-up examination, 66.6% (12/18) of the eyes that had gained VA one year after surgery maintained an improved VA (p=0.28), and 94.7% (18/19) of eyes that had achieved ambulatory vision at one year postoperatively maintained 20/200 or better (p<0.001). Evaluating the group of eyes that had a stable corneal surface one year after surgery, 93.9% (31/33) still had a stable corneal surface at the final follow-up (p=0.043).
At the final follow-up period, 81.8% (18/22) of the eyes maintained the improved corneal transparency when compared to the achieved in the first year after surgery, and 73.9% (17/23) of the eyes that had less corneal vascularization maintained a decreased corneal vascularization one year after surgery.
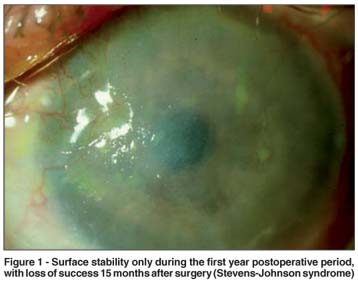
Group IIc had the poorest success rate (Figure 1).
Limbal graft rejection occurred in seven eyes (17.9%), four in haplo-identical HLA pairs, and three in identical HLA pairs; five of these seven eyes had an unstable surface after the rejection episode, one of which developed a descemetocele (case 6, group IIc). The seven eyes which developed limbal graft rejection needed a repeated lr-CLAL.
There was no statistical significant difference among groups of HLA pairs as regard limbal graft rejections (Table 3). Donor-recipient pairs with identical or 75% HLA match had, however, better clinical results than those with haplo-identity.
Infectious endophthalmitis occurred in one eye (case 4 of group IIc), one week after lr-CLAL, due to a persistent corneal epithelial defect and a secondary bacterial infection. This was due to Streptococcus pneumoniae, and besides intense topical and intraocular antibiotic therapy, therapeutic corneal transplant, lensectomy and posterior vitrectomy, this eye was lost.
The overall mean survival time for VA was 72.64 months (55.12 - 90.17 months, 95% CI) (Figure 2). The overall mean survival time for surface stability was 73.08 months (55.62 - 90.53 months, 95% CI) (Figure 3).
DISCUSSION
Allogenic limbal transplantation currently represents a reasonable technique and has been proven to be a successful treatment for patients with bilateral surface disorders, in whom the fellow eye is not healthy enough to be used as donor tissue(8-17).
The improvements achieved one year after surgery could be kept in the majority of patients at the long-term follow-up (mean, 48.7 ± 30.6 months) (Figure 4). Of the group of eyes that gained VA one year after surgery, 66.6% still maintained an improved VA, and 94.7% of eyes that have achieved ambulatory vision at one year after surgery maintained 20/200 or better at the final follow-up, similar to previous reports(20). In addition, of the group of eyes that had a stable corneal surface one year after surgery, 93.9% still had a stable corneal surface at the last follow-up, data confirmed on the survival curve. These parameters suggest a reasonable survival of stem cells at the long-term period after lr-CLAL.

However, the long-term follow-up reveals some loss in corneal transparency and some recurrence of corneal new vessels, especially in cases of group IIc, which might be due to stem cell exhaustion in these cases(18). Similarly to other published series(19-20), group IIc had the poorest success rate.
Our long-term results of HLA-matched lr-CLAL in restoring the ocular surface in bilateral cases of limbal deficiency are similar to previously published clinical series of both non-HLA-matched cadaver donors(9,11,13,15,18,20) and HLA-matched living donors(16-17), both with systemic immunosuppression.
Nevertheless, it is difficult to compare our results with those of other reports because there is an enormous variety in the severity of surface alterations in these patients. Thus, it is appropriate to separate patients into different groups of diagnosis and disease severity(19) to better analyze and compare results. It would be also interesting to separate those patients receiving simultaneous amniotic membrane and/or corneal transplantation, but these diseases sometimes require a combined approach to improve the success in restoring vision and the ocular surface.
Several clinical studies have shown good results with limbal transplantation using the same surgical technique described previously by other authors(6,15-16). The surgical procedure we used in our series of patients was similar to that employed in other study(6), except for the fact that we obtained donor limbal tissue without peripheral keratectomy. More pronounced donor limbal deficiency was shown when peripheral keratectomy is performed in donor eyes(24). Since the results of limbal transplantation without donor peripheral keratectomy are similar to those performed without removing peripheral corneal tissue(14,17,25), we believe that conjunctival limbal removal without keratectomy should be a preferred technique, to avoid the possibility of inducing an iatrogenic limbal deficiency.
Most allogenic limbal transplantations use donor cadaver eyes, which required systemic immunosuppression, usually with cyclosporine. Using HLA-matched living donors might reduce the need for systemic immunosuppression, and consequently there would be no associated risk of oral cyclosporine side effects, such as opportunistic infection, kidney toxicity, hypercalcemia, hypertension, and lymphoproliferative diseases(26).
We had one case of infectious endophthalmitis in our series, secondary to a corneal ulcer. Infectious corneal ulcers were reported several months after keratolimbal allografts in immunossuppressed patients, from 7.7% to 13% of eyes(15,18,20), however without endophthalmitis. Finding a compatible HLA-matched donor might avoid systemic immunossuppression and might decrease this serious complication.
Since we used no systemic immunosuppression in all patients of this series, and because 54.3% of our patients had a haploidentical HLA donor, we anticipated a high incidence of allograft rejection. Surprisingly, limbal graft rejection occurred in only 7 of the 39 eyes (17.9%), similar to the incidence reported by other authors(12,17). In our series, five cases of lr-LCAL rejections occurred in haploidentical HLA pairs and four in identical HLA pairs, with no statistically significant difference (Table 3). Nevertheless, 2 of the 3 lr-CLAL rejections that occurred in identical HLA pairs were present in eyes of patients with severe Lyell syndrome, all belonging to group IIc, which is known for having the poorest success rate(19-20).
Since most of the rejection episodes in our series occurred after a repeated lr-CLAL and in patients of group IIc, we might need to consider systemic immunosuppression in these patients, as well as in cases of an HLA haploidentity or non-compatible donor, or when a corneal graft is also performed.
The multicenter Collaborative Corneal Transplantation Studies (CCTS) Research Group reported that survival of high-risk corneal grafts was not related to HLA compatibility(27). On the other hand, it is well established that the HLA system has a strong influence on the survival of vascular grafts, such as in kidney, heart and heart-lung transplantation. Considering that the conjunctiva is a vascular tissue, our results are in agreement with this rule.
This retrospective long-term study strongly suggests that lr-CLAL without donor peripheral keratectomy is an adequate method of treatment for patients with severe bilateral surface disorders, with a reasonable maintenance of initial results at the long-term follow-up. It should be noted, however, that this is a non-randomized retrospective study. Randomized studies with larger number of patients should be carried out to complete the establishment of outcomes for this method.
REFERENCES
1. Thoft RA. Conjunctival transplantation. Arch Ophthalmol. 1977;95(8):1425-7.
2. Kinoshita S, Friend J, Thoft RA. Biphasic cell proliferation in transdifferentiaton of conjunctival to corneal epithelium in rabbits. Invest Ophthalmol Vis Sci. 1983;24(8):1008-14.
3. Tseng SC, Tsai RJ. Limbal transplantation for ocular surface reconstruction - a review. Fortschr Ophthalmol. 1991;88(3):236-42.
4. Pellegrini G, Traverso CE, Franzi AT, Zingirian M, Cancedda R, De Luca M. Long-term restoration of damaged corneal surfaces with autologous cultivated corneal epithelium. Lancet. 1997;349(9057):990-3. Comment in: Lancet. 1997; 349(9064):1556.
5. Chiou AG, Florakis GJ, Kazim M. Management of conjunctival cicatrizing diseases and severe ocular surface dysfunction. Surv Ophthalmol. 1998;43(1): 19-46. Comment in: Surv Ophthalmol. 1999;43(5):468.
6. Kenyon KR, Tseng SC. Limbal autograft transplantation for ocular surface disorders. Ophthalmology. 1989;96(5):706-22; discussion 722-3.
7. Thoft RA. Keratoepithelioplasty. Am J Ophthalmol. 1984;97(1):1-6.
8. Weise RA, Mannios MJ, Vastine DW, Fujikawa LS, Roth AM. Conjunctival transplantation. Autologous and homologous grafts. Arch Ophthalmol. 1985; 103(11):1736-40.
9. Tsubota K, Toda I, Saito H, Shinozaki N, Shimazaki J. Reconstruction of the corneal epithelium by limbal allograft transplantation for severe ocular surface disorders. Ophthalmology 1995102(10):1486-96.
10. Tsubota K, Satake Y, Kaido M, Shinozaki N, Shimmura S, Bissen-Miyajima H, Shimazaki J. Treatment of severe ocular-surface disorders with corneal epithelial stem-cell transplantation. N Engl J Med. 1999;340(22):1697-703.
11. Tseng SC, Chen JJ, Huang AJ. Classification of conjunctival surgeries for corneal disease based on stem cell concept. Ophthalmol Clin North Am. 1990; 3:595-610.
12. Tsai RJ, Tseng SC. Human allograft limbal transplantation for corneal surface reconstruction. Cornea. 1994;13(5):389-400.
13. Holland EJ, Djalilian AR, Schwartz GS. Management of aniridic keratopathy with keratolimbal allograft: a limbal stem cell transplantation technique. Ophthalmology. 2003;110(1):125-30.
14. Kwitko S, Marinho D, Barcaro S, Bocaccio F, Rymer S, Fernandes S, Neumann J. Allograft conjunctival transplantation for bilateral ocular surface disorders. Ophthalmology. 1995;102(7):1020-5.
15. Tan DT, Ficker LA, Buckley RJ. Limbal transplantation. Ophthalmology. 1996;103(1):29-36.
16. Rao SK, Rajagopal R, Sitalakshmi G, Padmanabhan P. Limbal allografting from related live donors for corneal surface reconstruction. Ophthalmology. 1999;106(4):822-8.
17. Daya SM, Ilari FA. Living related conjunctival limbal allograft for the treatment of stem cell deficiency. Ophthalmology. 2001;108(1):126-33; discussion 133-4.
18. Ilari L, Daya SM. Long-term outcomes of keratolimbal allograft for the treatment of severe ocular surface disorders. Ophthalmology. 2002;109(7):1278-84.
19. Holland EJ, Gomes JA, Shwartz GS. Preoperative staging of disease severity. In: Holland EJ, Mannis MJ, editors. Ocular surface disease: medical and surgical management. New York: Springer-Verlag; 2001. p.149-57.
20. Solomon A, Ellies P, Anderson DF, Touhami A, Grueterich M, Espana EM, et al. Long-term outcome of keratolimbal allograft with or without penetrating keratoplasty for total limbal stem cell deficiency. Ophthalmology. 2002;109(6): 1159-66.
21. Mannis MJ. Immunosupression in corneal grafting. In: Brightbill FS, editor. Corneal surgery. Theory, technique, and tissue. St. Louis: CV Mosby; 1986. p.317-21.
22. Kim JC, Tseng SC. Transplantation of preserved human amniotic membrane for surface reconstruction in severely damaged rabbit corneas. Cornea. 1995; 14(5):473-84.
23. Everitt BS, Pickles A. Statistical aspects of the design and analysis of clinical trials. London: Imperial College Press; 1999. p.125.
24. Farah M, Marinho DR, Kwitko S, Kirst M, Mársico J, Roehe D. Corneal epithelial healing in rabbit eyes with partial corneal and conjunctival limbal deficiency. Inv Ophthalmol Vis Sci. 1998;(Suppl 3):84.
25. Rymer S, Burnier M, Marinho D, Kwitko S, Belfort Júnior R, Rohe D. Conjunctival and corneal-conjunctival limbal autologous transplantation in the treatment of alkali burn in rabbits. Arq Bras Oftalmol. 2002;65(2):161-70.
26. Amos DB, Pool P, Grier J. HLA typing. In: Rose NR, Friedman H, editors. Manual of clinical immunology. 2nd ed. Washington: American Society for Microbiology; 1980. p.978-86.
27. The Collaborative Corneal Transplantation Studies (CCTS). Effectiveness of histocompatibility matching in high-risk corneal transplantation. The Collaborative Corneal Transplantation Studies Research Group. Arch Ophthalmol. 1992; 110(10):1392-403. Comment in: Arch Ophthalmol. 1992;110(11):1517-8.
 Corresponding author:
Corresponding author:
Caio Augusto Scocco
Rua Saint Hilaire, 316/101
Curitiba (PR) CEP 80240-140
E-mail: [email protected]
Recebido para publicação em 08.07.2007
Última versão recebida em 25.09.2008
Aprovação em 23.10.2008
Trabalho realizado no Hospital de Clínicas de Porto Alegre da Universidade Federal do Rio Grande do Sul - UFRGS - Porto Alegre (RS) - Brasil.